“I’m excited that folks are returning to some form of a normal life, whatever that means,” said Heather Drummond, COVID-19 vaccine director at the Washington State Department of Health. Still, she said, “the COVID-19 prevalence data continues to just be challenging to monitor.”
Surveillance systems linked to wastewater are giving a clearer sense of COVID-19. Hospitalizations and deaths have been on the decline, but have not disappeared completely. “So we are very grateful for that,” said Drummond, crediting the vaccines, people who have gotten the shots, and doctors who have encouraged their patients to do so.
But it’s important to carry lessons learned over the past three years into this new phase of the pandemic, said Dr. Eric Chow, chief of communicable disease and epidemiology at Public Health — Seattle & King County.
“We’re, of course, at a very different place in the pandemic now than at any other phase in the past few years,” he said. “Across a number of different metrics, including hospitalizations and deaths due to COVID-19, we’ve seen decreases, which is certainly an encouraging sign and probably speaks to the fact that we’ve had a lot more immunologic experience.”
Hospitalizations and deaths are still occurring, said Chow, disproportionately among people at risk for serious illness: those age 65 and older and people with underlying medical conditions — including kidney disease, diabetes, heart disease and lung disease — or suppressed immune systems.
“The thing that I fear moving forward is that people will forget about those lessons learned during the COVID-19 pandemic, and dismiss COVID as an ongoing threat in the community,” he said. “And I think that that would be a huge loss of all the knowledge that we had acquired during the pandemic.”
That knowledge will be key in the months to come, according to experts like Chow — especially amid a busy summer travel season and into fall, when respiratory viruses are often at their peak.
Here’s some guidance from public health experts in response to the lingering questions many people have about COVID now and in the future. If your questions aren’t answered here, please fill out the form at the bottom of this page and we’ll do our best to add that information to this story.
When do you need to get your next vaccine? Will it have a different formulation?
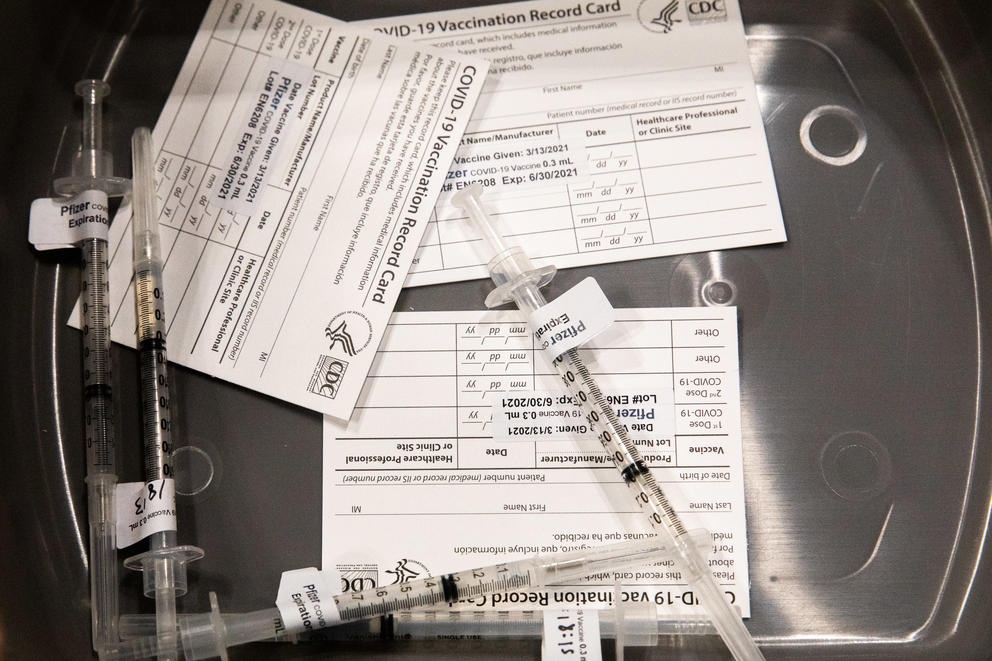
Guidelines from the Centers for Disease Control and Prevention can help determine your vaccine eligibility. In the spring, the CDC’s revised vaccine guidelines recommended that adults get one of the bivalent COVID-19 vaccines to be released in the fall. Older adults or immunocompromised folks were encouraged to consult with their doctors to determine whether to get a second dose of the bivalent vaccine.
Depending on when you’re due for your next shot, you could end up getting a different vaccine this fall. “What we are hearing from the CDC and other partners is that we can anticipate updated vaccination to be released and available to the public this fall, potentially in September,” said Drummond. “And so far most recommendations indicate that folks may be eligible for additional vaccination if it has been at least two months since their last dose.”
In June, the CDC and the U.S. Food and Drug Administration issued guidance for COVID-19 vaccine manufacturers to produce a new, targeted vaccine for this fall. This is standard practice for vaccines: The flu shot, for example, is reformulated every year to address the most common strains circulating.
Even if you’re planning to get one of the new vaccines in the fall, said Chow, it’s a good idea to check your vaccine status now and make sure you’re up to date for the summer, because people are still getting COVID and still getting sick enough to be hospitalized.
If you haven’t received the bivalent vaccine, he said, “now is the time to go ahead and get that, and this is especially important as people are thinking about travel plans for the summer … this is the best way to get that foundational immunologic protection.” As summer travel intensifies, he said, so do potential opportunities to contract and spread viral infections.
Will COVID vaccines continue to be free?
For now yes, regardless of insurance coverage, said Chow. This may change with the vaccines’ eventual commercialization, but Chow said federal stock would likely remain free and accessible through the end of the summer.
“Our expectation is commercialization will happen in tandem with the release of updated vaccines this fall,” said Drummond.
People with health insurance will get their vaccines paid for as they usually do, and the CDC and the Washington State Department of Health are working to reduce barriers for others.
DOH says it is making plans to circulate vaccines to underinsured or uninsured Washingtonians. The program will distribute vaccines through community health centers and federally qualified health centers at no cost to patients. DOH is also partnering with local pharmacies to do this. “We are working very hard to expand access as we prepare for COVID-19 vaccine commercialization so that anyone is able to receive a COVID-19 vaccine who wants one,” said Drummond.
The state Department of Health is providing COVID and flu vaccinations through mobile clinics. A schedule is available on DOH’s Care-a-Van website. This DOH site can help you find a place to get a vaccine.
How can I avoid long COVID?
Even a mild COVID infection can develop into a chronic condition. Long COVID can be debilitating, and we still don’t know much about it. According to Chow, risk factors and the burden of care for long COVID are both difficult to gauge, as is the number of people who develop it. “There’s some estimates out there [that] as much as 10% of people who recover from COVID go on to develop these longer-term symptoms,” he said. “But again, we’re still learning and this is something that we still need to invest more time to understand.”
Long COVID can arise even from mild infections, in people who may not otherwise have risk factors for developing serious illness. That’s something to keep in mind when evaluating when to take precautions, said Chow.
“There’s some evidence to suggest that for those people who stayed up to date with the recommended vaccines, the risk might be lower, but I think that we’re still trying to better understand what role vaccines play in the longer-term symptoms,” he said. “So ultimately it comes down to implementing those personal safety measures [like masking and ventilation] ... the standard steps we take to prevent infection in the first place.”
For those already infected with COVID, said Drummond, “working with their health care provider to potentially access Paxlovid or other medical countermeasures or resources can help to reduce the potential of having long COVID.”
Are super-dodgers real?
Three years in, some people seemingly still have not gotten COVID. Do they have a special immunity?
“It’s definitely possible,” said Chow. But it’s more likely that if you’ve avoided COVID for this long, it’s for another reason. Maybe you’ve taken serious precautions, kept up with vaccinations and simply avoided getting sick — or you did get COVID, but just never tested positive for it.
“It’s an important reminder that for some people, COVID comes in a variety of different severities. Some people will have asymptomatic infection,” he said. And if someone with a milder case hasn’t been regularly testing for it — and without symptoms, they would have little cause to do so — “they may not have ever known that they had the infection.”
What about non-pharmaceutical interventions?
While vaccines remain the primary tool in the ongoing public health effort to contain the spread of COVID-19, severe illness and death, non-pharmaceutical interventions like masking and improved ventilation are “something we encourage everyone to think about in terms of their level of risk tolerance,” said Drummond.
Mask mandates may be a thing of the past officially, but in crowded indoor spaces like airports, Chow said he would likely wear a high-quality, well-fitted KN95 or N95 mask.
“COVID-19 is likely here to stay with us for a long time, and it continues to circulate in the community,” he said. “And those same principles that we took into account to determine higher-risk situations for infection during the pandemic are still going to be true moving forward.”
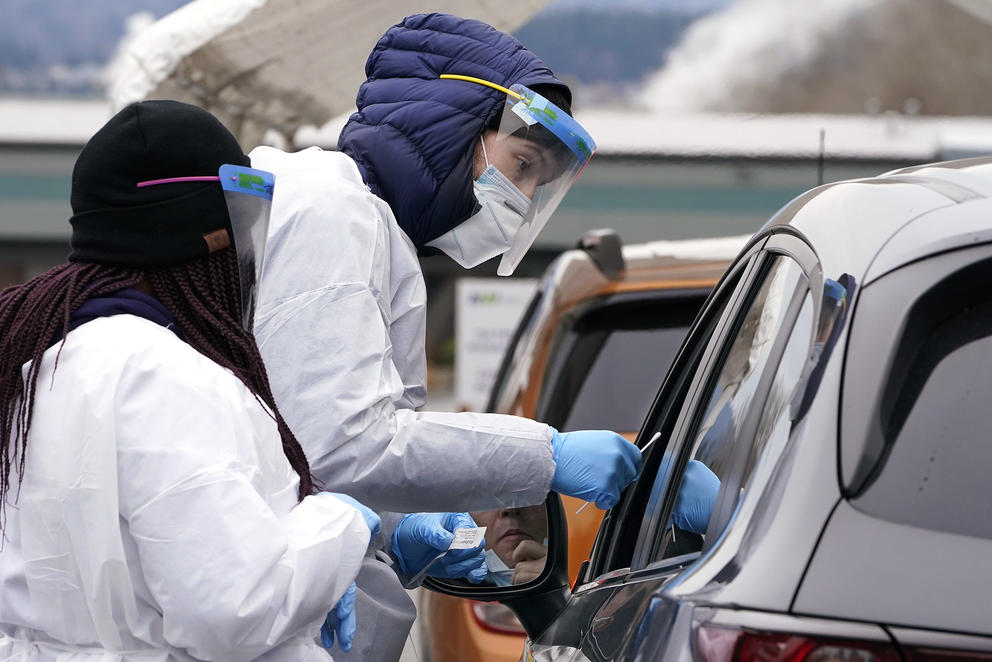
How are public health agencies gearing up for the fall?
DOH’s Drummond said communication and vaccination plans are underway. “Everyone remembers how challenging last fall was during respiratory virus season with flu, COVID-19, and RSV, or respiratory syncytial virus,” she said. “We are looking to coordinate messaging to support folks in accessing flu vaccine and COVID-19 vaccine to reduce their risk for severe disease during the fall.”
Vaccines will be the primary tool in preventing serious illness, hospitalization and death. “We are very concerned about the close circulation of COVID-19, flu, and RSV,” said Chow. “Just as we saw last year, they can surge in unpredictable ways, and so we are making plans, particularly around the vaccine front.”
For Public Health — Seattle & King County, this will take the form of community vaccination events and outreach to bring vaccines to people who are housebound or face other barriers to getting vaccinated during typical clinic hours. The goal is to boost vaccination rates before infection rates rise, said Chow. “That’s going to be ultimately our best protection against severe outcomes,” he said.
And for the future, Drummond said they’re watching for new COVID variants that may be more transmissible or more infectious.